Taking a Proactive Approach to RBQM Adoption
An environment of disparate clinical data, fragmented technology, and siloed resources are all barriers to adopting RBQM successfully.
- Disparate Clinical Data: Some of the challenges with RBQM adoption are due in part to a chaotic data environment. Though more data types and sources have created a richness in data sets that have benefited clinical research, they have also contributed to data chaos. Oftentimes, various data types and sources are stored in disparate systems, resulting in data variability, manual processes, and disjointed workflows between clinical teams. With system and data chaos, there has been a reluctance to adopt RBM / RBQM solutions as they have historically been considered yet another system to manage.
- Fragmented Technology: Another RBQM adoption challenge is rooted in technology. For an RBQM application to effectively assess and mitigate risk, it relies on a robust data pipeline to do so. RBQM as a point solution requires significant and oftentimes manual work by clinical teams in order to export, assemble, and then integrate disparate data sources within the solution. These inefficient, manual processes increase room for error and do not allow for a real time, holistic view of the data. Without accurate data that is being continuously refreshed, an RBQM application is less effective, leading to incomplete, non-contemporaneous data insights and delayed risk assessments, causing trial rework, delays, and potential risk to participants.
- Siloed Resources: Additionally, clinical teams that support risk-based quality management — typically data management and central monitoring teams — are often siloed. With organizational silos, clinical teams are often working in different systems to perform data mining, statistical analysis, and other due diligence required for RBQM. As a result, the probability of manual error increases and trial timelines are hindered. To address and overcome these challenges, sponsors must take a holistic approach to RBQM with an integrated, comprehensive technology solution.
Applying a Holistic RBQM Strategy
Taking a holistic approach to RBQM adoption — understanding how technology, processes and people are key parts of the overall strategy — positions life sciences organizations for more efficient monitoring and improved outcomes while complying with regulatory recommendations.
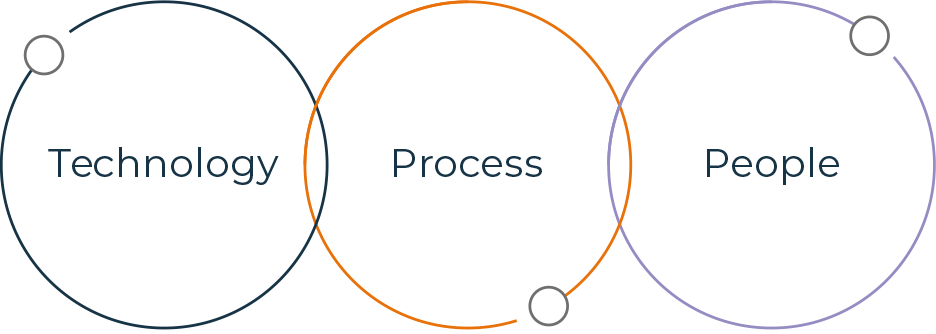
When developing an RBQM strategy, these components are essential considerations:
- Modern Technology: Moving at “the speed of science” means having clinical data available in near-real time to make decisions with confidence and accuracy — leveraging modern technology is essential in order to move at this pace. Rather than working in multiple systems to manage and monitor clinical data, a future-forward clinical data platform provides a single source of truth where all data can be collected and reviewed in near real-time. A modern platform not only reduces manual efforts, optimizes resources, and enhances productivity throughout the clinical trial lifecycle, but it provides a data-rich environment necessary for efficient risk assessment and identification. A data-rich environment feeds Key Risk Indicators (KRIs) to provide comprehensive risk profiles and a more holistic view of risk, enabling a data-driven monitoring effort and active oversight. Additionally, this complete view across all study data provides better visibility into the status of the study for all stakeholders across an organization.
- Automation & Process Optimization: Once all study data is integrated into a centralized location such as a clinical data platform, risk can be identified and assessed on an ongoing basis. To address risks efficiently, an ideal RBQM solution includes the ability to automate recommended actions based on risk-level or as threshold limits are being reached. Automated actions within a single system creates a seamless workflow across clinical teams, ensuring appropriate quality oversight throughout the duration of a clinical trial.
- Cross-functional Collaboration: Depending on the size of a life science organization, the traditional data management, clinical monitoring, and data science roles are often converged. This intersection of clinical functions creates an even greater imperative for adopting an RBQM solution within a clinical data platform. When RBQM is part of a unified platform, all teams are working off the same data management workbench, strengthening communication and collaboration. Added value can be found within RBQM solutions that serve as advanced data management workbenches with access to advanced statistical methods and visualization capabilities that enable roles across clinical teams to support oversight efforts
Combined CDR, ODR and MDR enables use cases across the clinical development value chain.

Implementing a Risk-Based Approach
As innovation in clinical development accelerates and more data than ever is being created from an expanding set of sources — from wearables to genomics — the complexity of clinical data and metadata management — and the impact of RBQM on trial monitoring practices — will continue to increase.
Regardless of how much the industry evolves, ensuring study integrity and patient safety will remain core priorities in clinical research. Leveraging the right technology will not only ensure that these objectives are achieved but will also provide an opportunity to streamline processes and increase operational efficiencies across clinical teams.
To learn more about taking a proactive approach to RBQM Adoption, download our latest white paper Establishing a Foundation for a Holistic RBQM Strategy.